What We Solve
Addressing the Problems that Break Access across the Aging Care Continuum
Access does not fail at enrollment.
It fails in execution — at predictable points across the care continuum.
Supply Chain Butler focuses on the problems that matter most, where cost escalates, responsibility concentrates, and outcomes are decided.
These problems repeat across markets, models, and geographies — which is why orchestration matters.

Across aging care, the same failure signals
appear again and again.
Wounds that Escalate
Missed Care Due to Logistics Breakdowns
Medication Complications & Falls that Compound Risk and Destabilize Care
Transitions that Fracture Accountability
These are not isolated problems.
They are symptoms of systems that were never designed
for longitudinal accountability at scale.
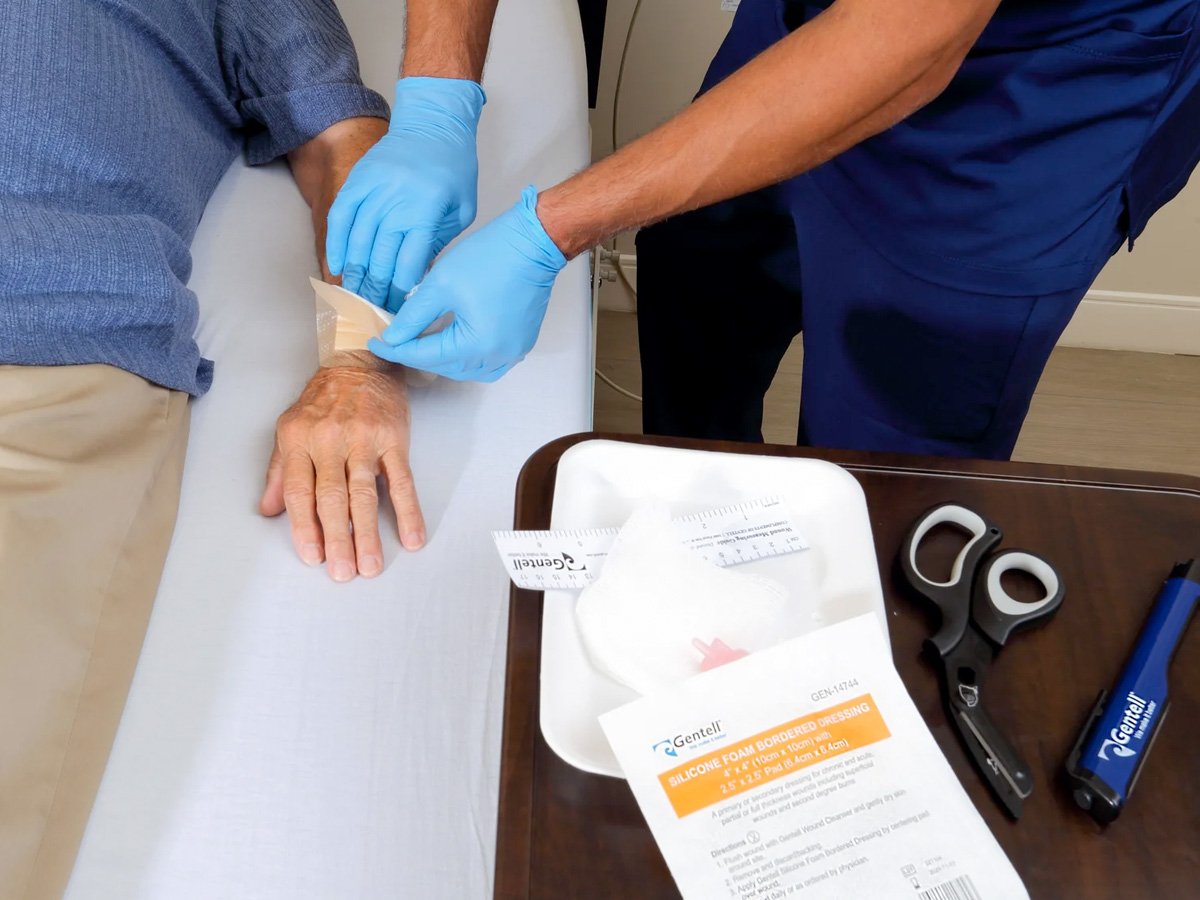
Wound Care Escalation & Avoidable Acute Spend
Wound care is one of the fastest paths to avoidable acute spend. What begins as a manageable clinical issue too often escalates due to fragmented protocols, delayed intervention, and misaligned incentives. By the time escalation occurs, cost has already shifted downstream.
Why It Matters Now
- Aging populations present with higher wound risk
- Post-acute settings carry the longest exposure window
- CMS accountability now extends across outcomes, not episodes
How This Shows Up:
Rehospitalizations
Extended Length of Stay
Margin Erosion
Higher Staff Burden

How We Address It:
We treat wound care as a system problem, not a supply problem.
Through coordinated execution across assessment, monitoring, and cost control, care is stabilized before escalation occurs.
Representative Capabilities
- Advanced wound care optimization
- Negative pressure therapy cost control
- Monitoring and early intervention support
 Get in Touch if
Get in Touch if
- Advanced wound care optimization
- Negative pressure therapy cost control
- Monitoring and early intervention support
Patient Logistics and
Missed Care Between Visits
Access fails when patients cannot reliably move through the system. Transportation gaps and missed visits quietly undermine care long before acuity rises.
Why It Matters Now
- Aging populations remain at home longer
- Rural and post-acute settings absorb downstream risk
- CMS rewards continuity, not activity

How This Shows Up:
Missed Appointments
Late Escalation
Avoidable Emergency Department Utilization

How We Address It:
Innovation plus Coordination
Logistics, coordination, and monitoring are orchestrated together to keep patients inside the care pathway.
Representative Capabilities
- Non-emergency medical transportation
- Caregiver coordination
- Visit adherence support
 Get in Touch if
Get in Touch if
- Missed visits are common
- ED utilization is rising
- Access breaks down between encounters
Medication Complexity, Polypharmacy & Falls Risk
Medication risk compounds silently over time. Polypharmacy, poor reconciliation, and limited visibility create instability that often presents first as falls, then escalates into hospital admissions and adverse events.
Why It Matters Now
- Higher acuity aging populations
- Longer care duration
- Increased regulatory and financial exposure

How This Shows Up:
Falls and Functional Decline
Adverse Drug Events
Avoidable Admissions

How We Address It:
Medication management is treated as a longitudinal system, not a point-in-time task.
Clinical risk, medication risk, and falls / functional risk are assessed together to create a defensible baseline and track change across the full care journey.
Representative Capabilities
- Medication intelligence and reconciliation
- Longitudinal clinical records
- Risk and functional status assessment
 Get in Touch if
Get in Touch if
- Falls are increasing
- Medication lists are complex
- Adverse events are difficult to predict
Care Transitions That Fracture Accountability
Transitions are where accountability most often breaks. As patients move across settings, information fragments, clinical context is lost, and responsibility diffuses.
Why It Matters Now:
- Aging populations move across settings more frequently
- CMS expectations span the full journey, not isolated episodes

How This Shows Up:
Incomplete or Missing Records
Repeated Assessments and Duplicative Work
Family Frustration and Loss of Trust
Readmissions driven by gaps in historical context

How We Address It:
Transitions are designed,
not improvised.
Continuity is preserved by maintaining a single, longitudinal view of the patient record that follows the individual across settings, providers, and episodes of care.
Representative Capabilities
- Longitudinal record consolidation
- Transition coordination
- Family and caregiver visibility
 Get in Touch if
Get in Touch if
- Readmissions follow discharge
- Care teams lack historical context
- Families struggle to understand the full care story
Start the Conversation
If you are navigating rising acuity, tighter margins, and expanding accountability, the question is no longer whether change is coming. The question is whether your execution model can support the scale and complexity already on the horizon.
If the responsibility sits with you, we’re ready to talk.

